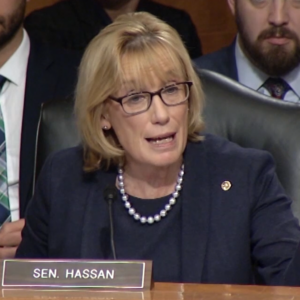
A Washington, D.C.-based group called Majority Forward is running a new ad that celebrates U.S. Sen. Maggie Hassan’s work to pass a law called the No Surprises Act in 2020.
“Maggie [Hassan] brought together Republicans and Democrats and passed a law that bans surprise medical bills,” says the woman featured in the ad, Andrea from Hopkinton. She certainly does deserve credit for her work on the No Surprises Act. Hassan, a Democrat, partnered with Louisiana Sen. Bill Cassidy, a Republican and a physician, to spearhead the No Surprises Act legislative success story.
As the ad says, the new law bans the surprise medical bills that occur when a patient seeks treatment believing it to be covered under their insurance plan, only to learn that one or more of the providers is not, in fact, covered.
The result is usually a huge bill you thought your insurance would take care of and an even bigger headache. Hassan’s bill will help patients save thousands of dollars in surprise costs.
The No Surprises Act made it so that patients would be left out of any billing disputes between healthcare providers and insurance companies. Those two parties are now required to seek arbitration through a fair and independent dispute resolution process. Both sides are incented to make an honest, reasonable offer because the arbitrator can only choose which of the two offers they believe is most fair. If the insurance company shoots too low, or if a provider asks for too much, the arbitrator might give them a rude awakening.
That’s how it’s supposed to work, anyway.
When the federal Department of Health and Human Services set about drafting the regulatory rules around the new law, however, it inserted a “benchmarking” provision that Congress specifically rejected. This provision would have established a median benchmark reimbursement rate for procedures and treatments. The big insurance companies loved this idea – indeed they lobbied Congress heavily for it – because it essentially allowed them to set reimbursement rates for out-of-network billing disputes. The lower they reimburse medical providers, the lower the median benchmark the higher the profits for Big Insurance.
As noted, Congress specifically rejected this model because of its far-reaching potential consequences. For example, if rural providers cannot earn fair and just compensation, they would have no option but to relocate. “More than 500 rural hospitals in the U.S. are at immediate risk of closing because of financial losses and lack of financial reserves to sustain operations, according to a report from the Center for Healthcare Quality and Payment Reform,” writes Ayla Ellison of Becker’s Hospital CFO Report.
Fortunately, a federal judge struck this rule from the law in February and ordered HHS to rewrite it to comply with Congressional intent. “The Rule conflicts with the unambiguous terms of the Act,” the judge wrote, adding that, “the Departments improperly bypassed notice and comment in implementing the challenged portions of the Rule.”
Now HHS must rewrite the rule. Hassan should protect her legislative legacy by urging HHS Secretary Xavier Becerra to rewrite it while honoring the clear intent of her legislation to protect patients and fairly compensate our cherished healthcare providers.